Deep Venous Disease
The deep venous system returns blood from the arms and legs to the heart. The veins are not under pressure like arteries, the blood flow passively being pumped by the action of the muscles in the arms and legs. One way valves in the veins prevent back flow and pooling of blood in the limbs. Any narrowing or blockages of the deep veins slows down the flow of blood, which can lead to problems for the arms and legs.
The hold up of blood can lead to swelling and discomfort of the affected limb. This back pressure can cause the valves in the veins to fail, which worsens the problem. Prolonged poor venous blood flow can cause the following problems:
- Leg swelling
- Leg pain
- Throbbing and aching sensations in your legs
- Skin becomes red or warm to touch
- Legs feel heavy
- Enlarged or varicose veins
- Ulcers on your feet, ankles, and lower legs
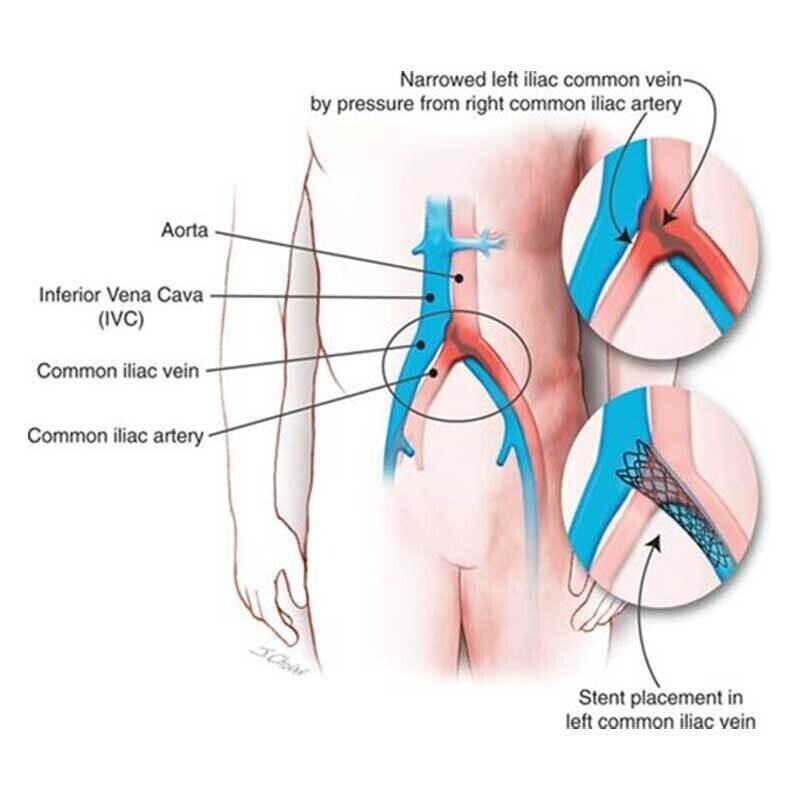
May Thurner Syndrome: left iliac vein compressed by the overlying artery
The slow blood flow can also lead to blood clots forming in the arms or more commonly the legs, called a Deep Vein Thrombosis (DVT). This can cause sudden swelling of the limb. There is also a danger of the blood clot breaking off and travelling to the lungs, known as a Pulmonary Embolus (PE). This is a medical emergency and can be life threatening.
In the longer term the DVT scars and narrows the vein resulting in worse flow of blood, more swelling, skin changes and eventually ulceration. This is known as ‘Deep Venous Insufficiency’ and ‘Post Thrombotic Syndrome’.
A common place for the deep vein narrowing is left common iliac vein, which is in the pelvis at the top of the left leg. The vein is compressed between the overlying right iliac artery and the bones of the pelvis behind them. This is also called ‘May-Thurner Syndrome’.
The vein narrowing of May-Thurner Syndrome is quite a common finding and doesn’t cause problems in most people. For some patients it may cause mild swelling of the leg for many years, but more commonly it suddenly causes a DVT with swelling and pain of the leg. The DVT can be diagnosed with ultrasound, CT and MRI.
Deep Venous Treatments
Traditionally the DVT was treated with elevation of the leg and blood thinning medication like warfarin. The clot would partially resolve and the swelling would improve, however often the long term problems of post thrombotic syndrome would develop.
For large DVTs, if detected early enough, the best treatment to avoid or reduce long term complications is to dissolve the DVT with a clot busting infusion (thrombolysis). Once the clot is cleared, the underlying vein narrowing can be opened up with a balloon and a stent that restores normal blood flow.
When there is a narrowing but no blood clot either from May-Thurner Syndrome or a previous DVT, a stent can also open this up to improve leg swelling and prevent post thrombotic syndrome.
Narrowings can occur on either side of the pelvis and also in the main vein back to the heart (inferior vena cava – IVC). All of these narrowing are potentially treatable with a stent to improve blood flow.
Deep venous stenting is a minimally invasive procedure usually performed under general anaesthetic. The procedure is guided by low-dose real-time X-ray imaging and intravascular ultrasound (IVUS – an ultrasound scan inside the vein). The whole procedure is performed through a tiny 2mm cut in the skin. Most patients go home the same day or the following day.
With his vascular surgeon colleagues, Dr Burfitt started the deep venous stenting service at Imperial in 2010. Over this period he has treated 100s of patients with deep venous problems and is one of the most experienced experts in the UK.


