Prostate Artery Embolization (PAE)
Prostate Artery Embolization is a low-risk minimally invasive procedure blocking the blood supply to the prostate gland, causing it to shrink down and thereby effectively treating urination problems, avoiding invasive surgical procedures and associated complications.
Dr Burfitt is one of the leading experts performing Prostate Artery Embolization (PAE) in London, treating patients in the NHS and private sector since 2015 when PAE was first introduced in the UK.
PAE Quick Summary
Trouble peeing?
Poor flow?
Got to go now!
Can’t start, can’t stop?
Repeatedly up in the night?
Know where every loo is when going out?
Can’t leave the house?
Concerned about TURP & Holep side effects?
Don’t want a urinary catheter?
Want to maintain sexual function?
Suddenly gone into retention?
Recurrent bleeding from the prostate?
- Minimally invasive – blocks blood supply, shrinking the prostate
- Treats underlying cause and preserves normal anatomy
- Sexual function maintained, no ‘dry orgasm’, no impotence
- No incontinence
- Painless – performed under twilight sedation, no general anaesthetic needed
- No surgical instruments through the penis
- Day case procedure – go home the same day
- No urinary catheter for procedure or when going home
- Quick recovery, 3-7 days
- 85-90% successful improvement in BPH symptoms
- Low level of complications, less than 1%
- Treats prostate size from 50cc to 400cc
- Good for medically unfit patients and those on blood thinners
- Works well for long-term indwelling catheter patients – a challenge for traditional surgery
PAE: THE FULL STORY
What is the Prostate Gland?
- Only found in men
- Size of a walnut – about 25 cubic centimetres (cc) in your 20s
- Sits below the bladder and just above the base of the penis
- Surrounds the first part of the tube (urethra) that carries urine from the bladder along to the end of penis.
- Gets bigger with age – 50cc, 100cc, 200cc, even 300+cc
- Two parts - inner central or transitional zone - TZ (where BPH enlargement occurs) and an outer peripheral zone - PZ (where most prostate cancers are found)
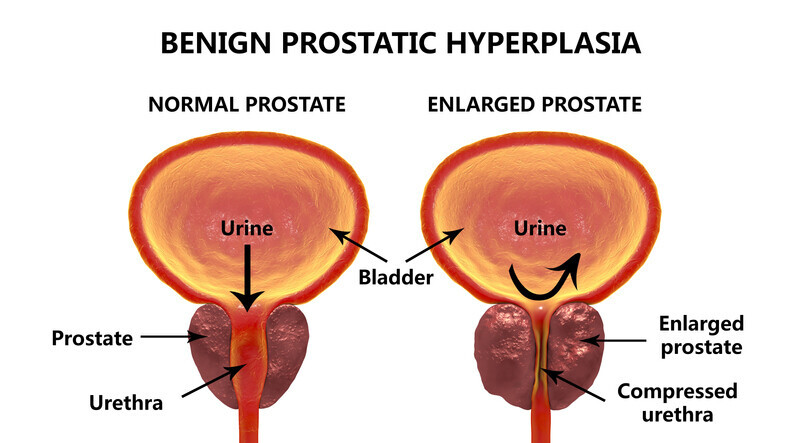
What is BPH – benign prostatic hyperplasia?
Non-cancerous enlargement of the prostate gland. Enlargement occurs in the central part - transitional zone.
At 20 years old the prostate gland measures around 25 cubic centimetres (cc), the changes of BPH can be seen in the late 30s and 40s. Once the prostate gland reaches over 40cc problems with urinating may start to occur. The gland can enlarge to over 300cc.
The causes of BPH are not clear, risk factors include:
- family history
- western diet
- obesity
- type 2 diabetes
However it often occurs in completely healthy men.
The underlying mechanism of growth seems to be the conversion of the hormone testosterone to dihydrotestosterone (DHT) locally within the prostate. DHT promotes growth of the normal prostate gland cells.
Symptoms of an enlarged prostate
Known as Lower Urinary Tract Symptoms (LUTS), they are caused by the enlarged prostate gland narrowing and obstructing the urethra carrying urine through the prostate gland from the bladder.
There two are groups of symptoms:
Storage symptoms
- Frequency - need to go more often during the day
- Urgency - I need to go now! Can even lead to incontinence
- Nocturia - repeatedly up at night to urinate – 3,4,5,6,7 times per night
Obstructive symptoms
- Low flow when urinating
- Hesitancy - difficulty starting to urinate
- Dribbling - takes a long time to finish urinating
- Incomplete emptying - feels like there’s still urine in the bladder after urinating
- Straining to pass urine
- Complete obstruction - suddenly unable to pass urine at all, this is a medical emergency that requires insertion of a tube through the penis into the bladder to drain the urine – urinary catheter
BPH and LUTS can seriously reduce a man’s quality of life, affecting work and leisure activities. It can also restrict sufferers to staying at home or only going out to places where they know there are lavatories on the way.
Urinary symptoms may also be related to bladder function - irritable bladder or bladder failure.
What is Prostate Artery Embolization (PAE)?
PAE is a low-risk minimally invasive non-surgical treatment that blocks the blood supply to the prostate gland, causing it to reduce in size. Consequently, the underlying problem of BPH enlargement is targeted, improving urinary function and preserving normal anatomy.
In the UK PAE has been recognised by NICE (National Institute of Clinical Excellence) since April 2018 as one of the standard BPH treatments. PAE is a painless procedure under local anaesthetic and twilight sedation, a general anaesthetic is not needed. PAE is generally done as a daycase, so you go home the same day, no overnight hospital stay is required.
Ultrasound and high resolution low-dose real-time X-ray imaging are used to accurately guide the embolization. No surgical instruments are passed through the penis, also a urinary catheter into the bladder is not required for the procedure or for going home.
The recovery is quick – expected side effects usually last 3 to 7 days. PAE does not cause incontinence, and there are no adverse effects on sexual function such as retrograde ejaculation or impotence. Improvement in symptoms start at around 2 to 3 weeks continuing to 3 months +. PAE is suitable for prostate sizes from 50cc up to 400cc
Suitable treatment for:
- Preserving sexual function
- Avoiding any incontinence
- Quick recovery
- long term indwelling catheter patients – normally challenging cases for surgery
- Patients taking blood thinners
- Patients unfit for general anaesthetic
- Large prostate glands – up to 400cc successfully treated
During PAE, under low-dose real-time X-ray imaging, a tiny tube called a microcatheter is manipulated from an entry point at the groin or the wrist to the prostate artery on one side within the pelvis.
The safe position of the microcatheter tip within prostate artery is confirmed by injecting a dye that shows up on X-ray and taking a specialized 3D image called Cone Beam CT (CBCT), this is the gold standard for knowing the exact correct position for the embolization.
Following this, tiny polymer beads measuring 250 or 400 microns in size are carefully infused through the microcatheter. The tiny beads flow with the blood down the prostate artery and block the very small arteries within the prostate by effectively silting them up.
Once one side is completed, the microcatheter is manipulated to other side, usually from the same access point and the process repeated to fully treat both sides of the prostate.
Blocking the arteries starves the prostate of blood causing it to shrink, also some central areas are killed off and reabsorbed, both of which reduce the overall size of the prostate gland. This reduction in size relieves the narrowing of the urethra, improving the flow of urine.
Another effect is to reduce the muscular tone within the prostate which also helps reduce the symptoms of BPH.
What are the advantages of PAE?
- Minimally invasive
- Treats underlying cause
- Painless procedure – performed under local anaesthetic and twilight sedation
- No general anaesthetic
- No surgical instruments through the penis
- Day case procedure – go home the same day
- No urinary catheter for procedure or when going home
- Quick recovery, 3-7 days
- Sexual function preserved, no retrograde ejaculation (‘dry orgasm’)
- No impotence
- No urinary incontinence
- 85-90% successful improvement in BPH symptoms
- Low level of complications, less than 1%
- Treats prostate size from 50cc to 400cc
- Good for medically unfit patients and those on blood thinners
- Works well for long-term indwelling catheter patients – a challenge for traditional surgery
- Effective treatment for acute urinary retention
- Used to stop recurrent bleeding from the prostate gland
PAE patient experience
What tests are needed?
We will arrange an outpatient with Dr Nick Burfitt at The London Clinic to fully discuss PAE and carry out the following tests all at the same visit:
International Prostate Symptom Score (IPSS) – a questionnaire giving a score to indicate the severity of your symptoms – mild, moderate, severe. You can take the IPSS test on-line by following this link: www.uptodate.com
Bladder ultrasound and flow test – measures the maximum and average flow rate when you pass urine, also measures how much urine is left in your bladder at the end of urinating - known as post-voiding residual (PVR)
CT angiogram (CTA) – a non-invasive CT scan that gives detailed 3D images of the pelvis. This shows the size and shape of the prostate gland, also whether the arteries are suitable for PAE. In addition it provides a ‘roadmap’ of the prostate arteries for the PAE procedure.
Urine sample test – to check for infection in the urine and bladder. Any infection would be treated with antibiotics before the PAE.
Blood tests – routine checks before doing the PAE (clotting, full blood count, urea and electrolytes)
Prostate specific antigen (PSA) - a blood test to screen/exclude prostate cancer. If your doctor has done this recently we don’t need to repeat it. Click here for more information about PSA
At this appointment we tell you if you are suitable for PAE, answer all your questions and if you are ready to go ahead, book a PAE date.
Who will be doing the PAE?
PAE is performed by an Interventional Radiologist (IR).
IRs are trained and certified in minimally invasive image-guided techniques such as embolization. They are also certified in the interpretation of the ultrasound, CT and MRI imaging needed to diagnose BPH and prostate cancer.
Your PAE will be performed by Dr Nick Burfitt, Interventional Radiology Consultant.
Dr Burfitt became a consultant in 2007 at Imperial College NHS Healthcare Trust, specializing in embolization & IR techniques throughout the body.
Dr Burfitt is one of the leading experts performing PAE in London and the UK.
Following training in Lisbon, Portugal with the pioneer of PAE Professor João Pisco, Dr Burfitt started the PAE service at Imperial in 2015, contributing cases to the Registry Of Prostate Embolization UK (ROPE-UK), the success of which led to NICE (National Institute of Clinical Excellence) recognition in 2018 of PAE as one of the standard BPH treatments in the UK.
For more information about Dr Nick Burfitt click here.

Where will the PAE take place?
In the Interventional Radiology Department at The London Clinic, Devonshire Place, London.
PAE is performed in a dedicated image-guided operating theatre. Whilst Dr Burfitt is performing the PAE, you will be carefully monitored and cared for by the specially trained IR nursing staff.
A Radiographer will also be present to control the imaging equipment.
How do I prepare for my PAE?
Do not eat for 6 hours beforehand, it is ok to drink clear liquids (water, squash, tea and coffee without milk) up to 2 hours before the procedure.
Please take your regular medications as normal with a sip of water.
What actually happens during PAE?
We will get you comfortable lying on the image-guided operating table.
The nurse looking after you will give you an intravenous sedative to make you feel relaxed and also an antibiotic to prevent any infection.
Your blood pressure, heart rate and oxygen levels will be monitored closely throughout the procedure. Depending on the artery access point, the skin over the groin or wrist will be cleaned and sterile drapes placed over you.
Local anaesthetic will be injected through a fine needle under the skin and down to the artery, this will sting a little for about a minute and then go numb.
A small access tube (less than 2.5mm in diameter) will be carefully inserted into the artery under ultrasound guidance, once this is in position you will not really be aware of what is happening inside the arteries.
A very tiny tube called a microcatheter (0.7mm in diameter) is then manipulated under real-time low-dose X-ray into the prostate artery on one side.
The correct position of the microcatheter tip within the prostate artery will be confirmed by injecting a dye which shows up on X-ray and taking a specialized 3D image called Cone Beam CT (CBCT), this is the gold standard for confirming the exact correct position for the embolization.
Following this, tiny polymer beads measuring 250 or 400 microns in size are carefully infused through the microcatheter. The beads flow with the blood down the prostate artery and block the very small arteries within the prostate by effectively silting them up.
Once one side is completed, the microcatheter is manipulated to the other side, usually from the same access point and the process repeated to fully treat both sides of the prostate.
At the end of the PAE all tubes are removed. In the groin a very small collagen plug is placed at the artery access site to help stop any bleeding, your body absorbs the plug over the next few months. At the wrist, pressure is applied for about 20 minutes to the artery access site to stop any bleeding.
How long does the PAE take?
Most PAEs take about 2 hours of actual procedure time, sometimes longer - up to 3 hours, usually when there is more than one prostate artery on one side, or the angles to the prostate arteries are a bit tricky.

Does PAE hurt?
The local anaesthetic at the beginning of the procedure stings a bit for around 60 seconds, otherwise PAE is not a painful procedure.
Patients can sometimes get a bit uncomfortable lying on the operating table for a few hours, which is why we give intravenous sedation and painkillers, also known as ‘twilight sedation’ – patients often fall asleep during the PAE.
What happens after the PAE?
Once the PAE is completed, you will be transferred back to your private room on the ward for bed rest and observation for 4 hours. You can eat drink normally immediately after the PAE.
Before you go home, we ensure there is no bleeding from the artery access site and that you have passed urine.
We will send you home with a week’s course of antibiotics and pain killers.
You will have our contact details if there are problems or you want to ask any questions.
The expected side effects after PAE
Most patient experience one or two of the expected side effects for 3 to 7 days after the PAE, at the most 10 days.
The most common is a stinging sensation when passing urine (dysuria), this can be mild or sometimes quite severe, resulting in going to the bathroom and being up in the night more frequently for a few days. The painkillers you are discharged with will help with this.
Some patients may have a small amount of blood in the urine or from the back passage, this generally clears after a 3 to 5 days.
Occasionally patients get some blood in their semen on ejaculation causing a pink or light brown colour, this can last for a couple of months, but is not of concern.
Whilst you are on the ward after PAE, very occasionally (less than 5% of patients) cannot pass urine. If this happens we will insert a urinary catheter to empty the bladder. The catheter will stay in for 2 weeks to allow everything settle down and then removed.
All of the above are normal and expect side effects of PAE. You are unlikely to experience all of these side effects, but you are likely to get one or two for a few days.

Follow up after the PAE
Dr Burfitt will contact you by telephone 2 weeks after the PAE to see how you are doing.
At 3 months after the PAE, we will arrange an MRI of the prostate and an ultrasound bladder/flow test. This will be followed by a clinic appointment with Dr Burfitt to review the outcome of your PAE.
You will have our contact details if there are problems or you want to ask any questions at any time.
The possible complications after PAE
Occasionally there may be some bleeding from the artery access site at the groin or wrist which will cause bruising in the surrounding skin, sometimes a small collection of blood may form called a haematoma. The haematoma generally resolves by itself, but if it became large we would ask you to come back for review.
Whilst very uncommon, the main complication of concern is ‘non-target embolization’ - beads going somewhere other than the prostate, such as the bladder, bowel or penis which are all nearby.
This is very rare, occurring significantly less than 1% of the time. When it does occur, the problem usually resolves by itself and does not require another procedure.
The use of Conebeam CT during the PAE ensures we are in exactly the right place for embolization, non-target embolization has not occurred in any of Dr Burfitt’s patients to date.
PAE history and results
PAE was used as early as the 1970’s to treat the bleeding complications of prostate biopsy and surgery. In one of these patients, the improvement of BPH symptoms by PAE was noticed and reported in the scientific literature in 2000 [1].
In 2008 the first intentional treatment of BPH with PAE was performed by Dr Francesco Carnevale in Sao Paolo Brazil, with success in unblocking patients in complete urinary obstruction, there by getting rid of their urinary catheters.
Since that time PAE has spread around the globe with 10,000s of BPH patients being successfully treated Worldwide. Numerous published scientific studies report the successful outcomes of PAE at 85-90%, persisting on long term follow up (76.3% at 3 to 6 years) [3,4].
PAE also has a very low rate of significant complications at less than 1%. [3,4]
In comparison to TURP, a number of studies have demonstrated PAE has similar outcomes and quality of life improvements – but with shorter recovery and without the adverse effects on sexual function and possible incontinence of TURP. [5,6,7]
In patients with long term catheters, 94.6% success in catheter removal has been recorded, with 78% of patients being retention free at long term follow of 3 to 6 years.
Is BPH the same prostate cancer?
The short answer is no. BPH is over growth of normal non-cancerous prostate tissue.
It is possible to have BPH and prostate cancer at the same time. Men over the age of 45 or 50 should regularly have the blood test for prostate cancer done by their GP (see PSA test below). If there is any suspicion of prostate cancer, you will have an MRI scan of the prostate to look for cancer more closely. You may go on to have biopsies of the prostate depending on the appearances on the MRI.
The decision and possible treatment of prostate cancer would be under a Consultant Urologist, you may need to have surgery if there is a significant cancer present.
Many cancers are not of concern and surgery is not needed, these are kept under surveillance ‘watchful waiting’. Patients with a small un-concerning cancer and BPH can go on to have PAE for their urinary problems. It is quite common to treat these type of patients. In fact PAE may actually treat the cancer as well (although this is not a reason to have PAE).
More about the Prostate Specific Antigen (PSA) Test
The PSA test is done to look for the prostate cancer. PSA is a protein produced by prostate gland cells to make semen more liquid, it also goes into the blood. In the prostate the PSA is made by both normal and cancerous cell.
Causes of a raised PSA level are:
- The prostate gland is enlarged with Benign Prostatic Hyperplasia (BPH)
- Infection is present in the prostate gland - Prostatitis
- Urine infection - Urinary Tract Infection (UTI)
- Prostate cancer
A raised PSA does not necessarily mean you have prostate cancer. If your PSA is significantly raised, we will arrange tests to look for infection and an MRI to look for prostate cancer and refer you to a Urologist specializing in prostate cancer treatment.
References
1. DeMeritt J, Elmasri F, Esposito M, Rosenberg G. Relief of benign prostatic hyperplasia-related bladder outlet obstruction after transarterial polyvinyl alcohol prostate embolization. J Vasc Interv Radiol 2000;11(6):767-70.
2. Carnevale FC, Antunes AA, Da Motta Leal Filho JM, et al. Prostatic artery embolization as a primary treatment for benign prostatic hyperplasia: Preliminary results in two patients. Cardiovasc Intervent Radiol 2010;33(2):355-61.
3. João M Pisco 1 et al, Medium- And Long-Term Outcome of Prostate Artery Embolization for Patients With Benign Prostatic Hyperplasia: Results in 630 Patients. J Vasc Interv Radiol Aug 2016, 27 (8), 1115-22.
4. Schreuder SM, Scholtens AE, Reekers JA, Bipat S. The role of prostatic arterial embolization in patients with benign prostatic hyperplasia: a systematic review. Cardiovasc Intervent Radiol 2014;37(5):1198-219.
5. Carnevale FC, Iscaife A, Yoshinaga EM, et al. Transurethral resection of the prostate (TURP) versus original and PErFecTED prostate artery embolization (PAE) due to benign prostatic hyperplasia (BPH): preliminary results of a single center, prospective, urodynamic-controlled analysis. Cardiovasc Intervent Radiol 2016;
6. Gao Y, Huang Y, Zhang R, et al. Benign prostatic hyperplasia: prostatic arterial embolization versus transurethral resection of the prostate - a prospective, randomized, and controlled clinical trial. Radiology 2014;270(3):920-8.
7. Rassweiler J, Teber D, Kuntz R, Hofmann R. Complications of transurethral resection of the prostate (TURP)--incidence, management, and prevention. Eur Urol 2006;50(5):969-79; discussion 980.