Varicocele Embolization (VE)
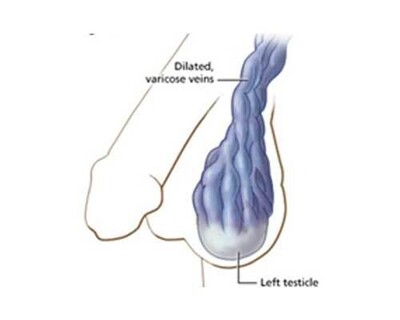
A varicocele is some enlarged or dilated veins in the scrotum (ball sack), caused by back pressure in faulty veins draining blood away from the testicles. They most commonly occur on the left side, but can be on both sides.
Varicoceles can cause an aching pain in scrotum. They are also associated with low sperm count and quality. In addition, varicocele can be a cause of low testosterone.
Varicocele Embolization is a non-surgical, image guided, minimally invasive procedure to block the back pressure in the testicular veins, relieving pain, improving sperm production and increasing testosterone.
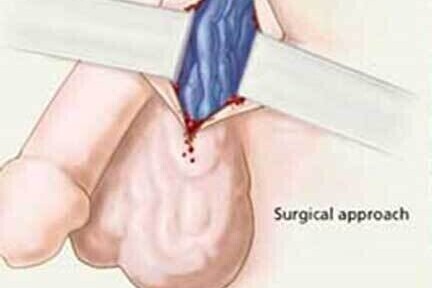
The traditional surgical alternate involves an incision in the scrotum or groin and tying off of the problematic veins, usually under general anaesthetic.
VE QUICK SUMMARY
Pain? - a dull ache to a stabbing pain
Pain worsens throughout the day or when standing?
Lumpy feeling in the scrotum?
Scrotum hanging low?
Visible enlarged veins in the scrotum?
low sperm count and poor sperm quality?
Low testosterone levels? ‘Low-T’
Smaller testicle on one side?
- Under local anaesthetic and ‘twilight’ sedation - no general anaesthetic
- Minimally invasive procedure under ultrasound and low dose real-time X-ray guidance
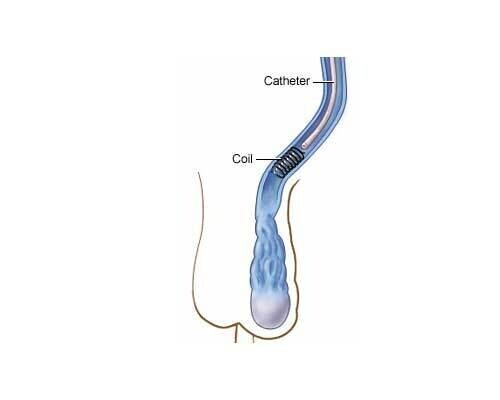
- The testicular vein is blocked with small platinum coils and a sclerosant
- Quick procedure – 30 to 45 minutes
- 1-2 hour recovery before going home
- No incision in scrotum or groin
- Return to work the following day
- Up to 50-60% pregnancy rate after embolization
- Over 90% technical success rate
VE: The Full Story
What causes a Varicocele?
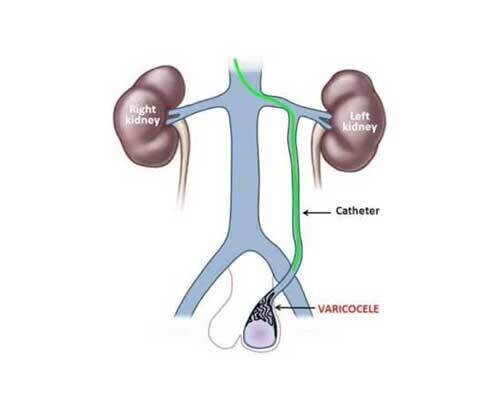
The veins from the testicles (known as the testicular or gonadal veins) pass up out of the scrotum, through the groin and up through the back of the abdomen (tummy). On the left side the testicular vein joins the vein from the left kidney. On the right side the it joins the main vein from the lower body (known as the vena cava) returning to the heart.
The testicular veins are thin walled, low pressure and the flow is ‘up hill’ back to the heart. When you are standing up, normal veins have one-way valves which prevent the back flow of blood. When a varicocele is present, the valves in the testicular vein are leaky or not present at all.
This means the testicular vein contain a standing column of blood, exerting hydrostatic pressure into the veins in the scrotum. This stretches the veins in the scrotum making them progressively bigger over time. (This is similar to varicose veins in the legs)

Normal valves and flow

Faulty valves and back flow
Left-sided varicocele
Varicocele Symptoms and Problems
The stretching of the veins in the scrotum can cause pain, especially after a long time standing up. The pain can be a dull ache, a heavy dragging sensation or sometimes quite a sharp pain.
The enlarged veins can be felt within the scrotum, almost like a ‘bag of worms’.
When they get really big they can be seen as unsightly bulging lumps in the scrotum with a blue-ish colour.

Varicocele and fertility
Varicoceles are present in 10-15% of all men and generally cause no problems. 40% of sub-fertile men have a varicocele. Also couples who have successfully had a child, but are having a difficulty conceiving a second time, the presence of varicoceles can be as high as 81%.
We know that varicocele is associated with reduced male fertility, but the exact reason is not completely clear, the cause is thought to be increased temperature of the testes and poor blood flow. The testicles need to a be a bit cooler than the body for normal sperm and testosterone production. This is why they are outside of the body in the scrotum and can move up and down, allowing regulation of their temperature.
The pooling of blood in a varicocele warms the testicles, reducing the number and quality of sperm produced.
In addition, the pooling of blood means waste products of metabolism are less efficiently cleared from the scrotum, which may also affect sperm and testosterone production.
When present from adolescence, a varicocele may cause one testicle to be smaller. Smaller testicles produce fewer sperm.
Early treatment of varicocele can allow a small testicle to grow to normal size.
Varicocele treatment improves fertility in around 50-60% of couples. Studies have shown 83% of patients have an increase in sperm production with embolization (versus 63% with surgical operation.)
Clearly reduced fertility has many causes, treating a varicocele eliminates one of the possible causes.
Varicocele and Testosterone
Testosterone, the male sex hormone, is produced by the Leydig cells in the testicles.
A number of studies have shown a link between varicocele and low testosterone. Similar to sperm production, the increased temperature of the testicle and poorer clearance of metabolites inhibits the Leydig cells resulting in them making less testosterone. This is the case even if the varicocele is not visible and there is no pain or symptoms. Testosterone levels get lower with age, however a testosterone level below 11nmol/l can lead to ’Low T’ symptoms:
- Problems with erections
- Low sex drive
- Reduced muscle mass
- Hair loss
- Reduced amount of semen
- Increased body fat
- Reduced energy levels
Varicocele treatment has been shown to increase testosterone levels by up to 25% and is an alternative to testosterone replacement therapy in patients with varicocele.
What is Varicocele Embolization (VE)?
VE is a minimally invasive, non-surgical procedure to block the veins draining the varicocele in the scrotum.
The procedure is performed under ultrasound and low-dose real-time X-ray imaging.
A small tube (less 2mm) is inserted into a vein in the side of the neck, from this position the testicular veins are blocked with a combination of tiny platinum coils and sclerosant liquid which sticks shut the veins, thereby stopping the back-flow. It is performed as a day-case procedure under local anaesthetic and twilight sedation, so you can go home 2 hours after the procedure.
Most patients go back to work the next day.
The surgical alternative to VE
The traditional surgical varicocele repair is performed under general anaesthetic, an incision is made in the upper scrotum or groin and the veins are tied off to stop the back flow. Patients may go home the same day or the following morning. Depending on your job, the return to work is 2-4 days. There is small a risk of infection in the wound, also collection of fluid around the testicle called a hydrocele.

Do all varicoceles need repair?
The short answer is ‘no’ – if the varicocele is not painful or unsightly, there are no problems with fertility and no symptoms of low testosterone, then there’s no need to have varicocele treatment. 10 – 15% of all men have a varicocele, in the majority it causes no problems.
What are the advantages of VE?
- Minimally invasive treatment that avoids incisions in the scrotum or groin
- Quick procedure with short recovery
- You can go home the same day
- Return to work the next day
- Very low risk
- When both sides are treated, it’s all done through the same access point, unlike surgery where incisions on both sides are required
- Treats varicocele pain effectively
- Shown to improve fertility
- A treatment for low testosterone, potentially avoiding testosterone replacement therapy (TRT)
Which tests are needed for Varicocele Embolization?
We will arrange an outpatient with Dr Nick Burfitt at The London Clinic. At this appointment, Dr Burfitt will also carry out ultrasound of the scrotum – this is to confirm the presence of the varicocele, see if it is on one or both sides, check for any other problems in the scrotum and the kidneys that could be causing your symptoms.
At this appointment we tell you if you are suitable for varicocele embolization, answer all your questions and if you are ready to go ahead, book a date for the embolization.
Who will be doing the Varicocele Embolization?
The embolization will be performed by Dr Nick Burfitt, Interventional Radiology Consultant.
Interventional Radiologists (IRs) are trained and certified in minimally invasive image-guided techniques such as embolization. They are also certified in the interpretation of the ultrasound, CT and MRI imaging.
Dr Burfitt became a consultant in 2007 at Imperial College NHS Healthcare Trust, specialising in embolization & IR techniques throughout the body and has been treat varicocele patients for 14 years.
Where will the embolization take place?
In the Interventional Radiology Department at The London Clinic or Cromwell Hospital in London.
Varicocele embolization is performed in a dedicated image-guided operating theatre. Whilst Dr Burfitt is performing the embolization, you will be carefully monitored and cared for by the specially trained IR nursing staff.
A Radiographer will also be present to control the imaging equipment.
How do I prepare for my VE?
Do not eat for 6 hours beforehand, it is ok to drink clear liquids (water, squash, tea and coffee without milk) up to one hour before the procedure.
Take your regular medications as normal with a sip of water.
What actually happens during Varicocele Embolization?
We will get you comfortable lying on the image-guided operating table. The nurse looking after you will give you an intravenous sedative to make you feel relaxed.
Your blood pressure, heart rate and oxygen levels will be monitored closely throughout the procedure.
The testicular veins are actually accessed by a vein in the right side of the neck (jugular vein). The skin over the vein is cleaned and sterile drape placed over you.
Local anaesthetic will be injected through a fine needle under the skin and down to the vein, this will sting a little for about a minute and then go numb.
A small access tube (less than 2.5mm in diameter) will be carefully inserted into the vein under ultrasound guidance, once this is in position you will not really be aware of what is happening inside the veins. A small tube called a catheter (less than 2mm in diameter) is then manipulated under real-time low-dose X-ray into the testicular vein. The correct position of the catheter tip within the testicular vein will be confirmed by injecting a dye which shows up on low dose X-ray.
Following this, small platinum coils are placed through the catheter into the testicular vein. A sclerosant fluid is also injected around the coils which sticks the vein shut. In combination the coils and sclerosant block the vein preventing back flow to the scrotum.
If there is a varicocele on both sides, from the same access point in the neck, the catheter is manipulated to other side, and the process repeated to fully treat both varicoceles. At the end of the embolization all the tubes are removed. Pressure is applied to the vein in the side of the neck for 5 minutes to stop any bleeding.
Is the procedure painful?
The local anaesthetic at the beginning of the procedure stings a bit for around 60 seconds.
You may get a dull ache in the tummy after the sclerosant is injected, which last for 10-20 mins, otherwise the embolization is not painful.
We will give you intravenous sedation throughout the procedure to keep you relaxed and comfortable.
What happens after the VE?
Once the embolization is completed, you will be transferred back to your private room on the ward for bed rest and observation for 2 hours. You can eat drink normally immediately after the embolization.
Before you go home, we ensure there is no bleeding from the vein access site.
You will have our contact details if there are problems or you want to ask any questions.
Follow up after the PAE
Dr Burfitt will contact you by telephone 2 weeks after the PAE to see how you are doing.
Generally the discomfort from the varicocele will resolve in the first month, but can take up to 3 months.
You may be able to feel the varicocele in the scrotum for quite a while after the embolization. Although the back pressure has been stopped, the veins have been chronically stretched for years, so take some time to shrink down.

Varicocele Embolization results
The technical success of the procedure is over 95%.
89% of men are reported to have relief of scrotal pain following embolization.
Varicocele treatment improves sperm count and quality in 60-80% of men. Successful pregnancy is reported in up to 50% of sub-fertile couples after VE.
In patients with low testosterone and a varicocele, embolization has been shown to raise testosterone levels by up to 25%.
What are the risks?
Varicocele embolization is a low risk procedure with complications significantly lower than 1%.
As with all procedures, there is a small risk of infection, this is significantly reduced compared to surgery as the embolization is minimally invasive.
There is no risk of fluid collecting around the testicle (hydrocele) which is can occur after surgery.
A very rare complication (less than 1 in 1000) of varicocele embolization is coil migration from the testicular vein to elsewhere in the body, usually the left renal vein or a vein in the lung. This happens at the time of the embolization, so the coil can be simply retrieved as part of the procedure, using the same access point in the neck.
Coil embolization is avoided by careful technique and proper oversizing of the coils to the testicular vein.
To date, coil migration has not occurred in any of the patients treated by Dr Burfitt.
References
Beneficial Effects of Varicocele Embolization on Semen Parameters Prasivoravong J et al. Basic Clin Androl. 2014 May 16;24:9.
Varicocele Repair Versus Testosterone Therapy for Older Hypogonadal Men with Clinical Varicocele and Low Testosterone. Bernie HL, Goldstein M.Eur Urol Focus. 2018 Apr;4(3):314-316.