What is pelvic congestion syndrome?
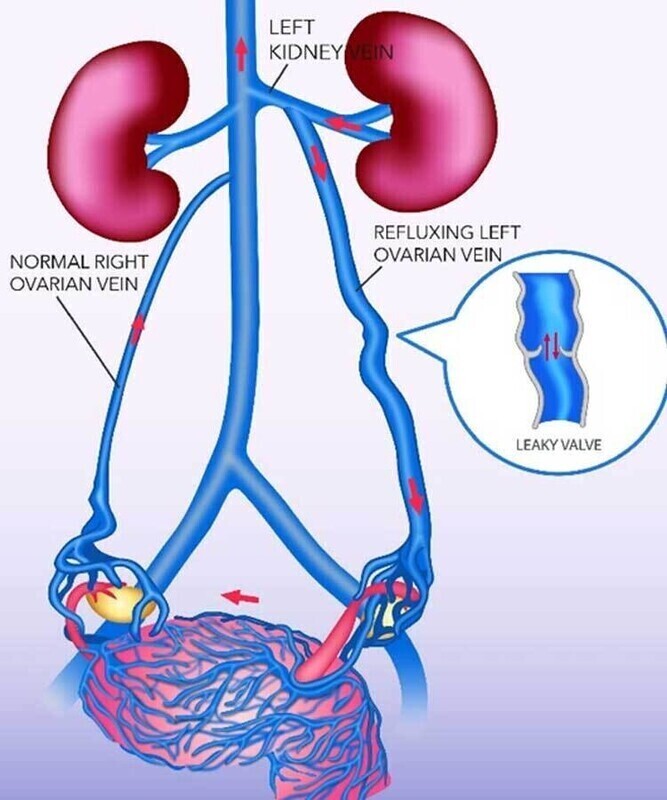
Pelvic congestion syndrome is a type of vascular disease that develops when the veins in your pelvic region don’t efficiently push blood back to your heart. As a result, your blood can pool in your veins and make them swell and bulge, much like varicose veins that form in your legs. Venous insufficiency usually develops when the small valves in your veins don’t function correctly, and your blood moves slowly or even flows backward.
Your risk of venous insufficiency increases if you’re overweight or pregnant. You have a higher chance of developing the condition if you have a family history of venous insufficiency or if you smoke. It also occurs in women who are otherwise completely healthy.
Pelvic pain in women can have many causes, in first instance the best person to talk to is a gynaecologist who can diagnose the cause of the problem. If you are suffering with pelvic congestion syndrome, they will refer you to an interventional radiologist who is expert in the minimally invasive technique of embolization used to treat pelvic congestion syndrome.
What are the symptoms of pelvic congestion syndrome?
Pelvic pain is the most common symptom of pelvic congestion syndrome. Your pain often worsens as the day goes on, especially if you have to stand or sit all day. You might also have pain during intercourse or severe menstrual cramping. Physical activities like horseback riding and bicycling can also trigger your pain.
How is pelvic congestion syndrome treated?
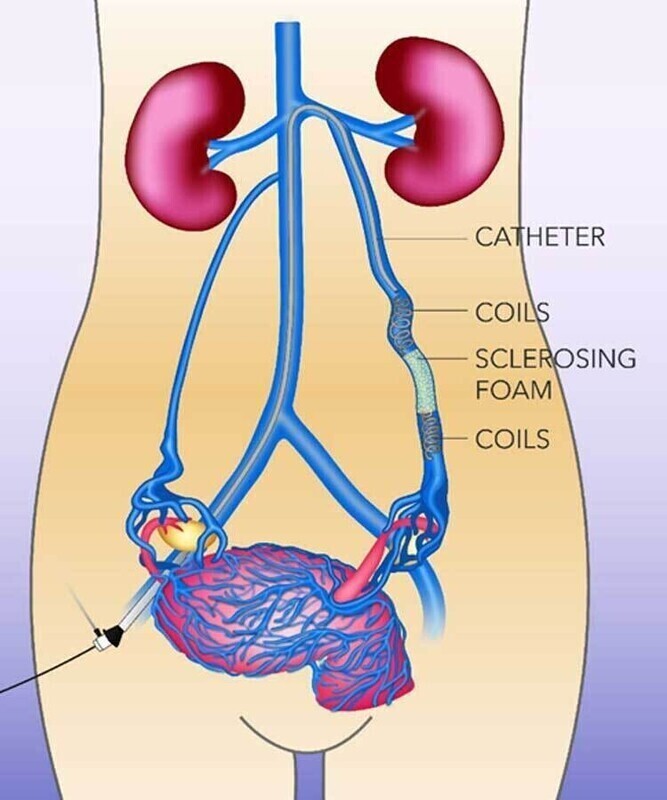
Pelvic congestion syndrome is treated by embolization which is a minimally invasive, non-surgical procedure to block the back-flow in the pelvic veins. The procedure is performed under ultrasound and low-dose real-time X-ray imaging.
A small tube (less 2mm) is inserted into a vein in the side of the neck, from this position the pelvic veins are blocked with a combination of tiny platinum coils and sclerosant liquid which sticks shut the veins, thereby stopping the back-flow. It is performed as a day-case procedure under local anaesthetic and twilight sedation, so you can go home 2 hours after the procedure. Most patients go back to work the next day.
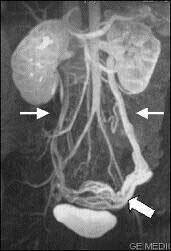
MRI image diagnosing enlarged pelvic veins
Which tests are needed?
An MRI scan confirms the presence and extent of the abnormal pelvic veins and also looks for other causes of the symptoms you are experiencing.
An internal ultrasound of the pelvis may also be needed which is done through vagina (transvaginal ultrasound). This shows which veins have the abnormal backward flow and allows us to target the problem veins during the embolization procedure.
We will arrange an outpatient appointment with Dr Nick Burfitt to fully discuss the test results and pelvic congestion syndrome. He will answer all your questions and if you are ready to go ahead, book a date for the embolization.
Who will be doing the Embolization?
The embolization will be performed by Dr Nick Burfitt, Interventional Radiology (IR) Consultant.
Interventional Radiologists (IRs) are trained and certified in minimally invasive image-guided techniques such as embolization. They are also certified in the interpretation of the ultrasound, CT and MRI imaging.
Dr Burfitt is a consultant at Imperial College NHS Healthcare Trust, he specialises in embolization & IR techniques throughout the body. He has been performing pelvic vein embolization since 2009.
Where will the embolization take place?
The embolization is performed in a dedicated image-guided operating theatre. Whilst Dr Burfitt is performing the embolization, you will be carefully monitored and cared for by the specially trained IR nursing staff.
A Radiographer will also be present to control the imaging equipment.
How do I prepare for my procedure?
Do not eat for 6 hours beforehand, it is ok to drink clear liquids (water, squash, tea and coffee without milk) up to one hour before the procedure.
Take your regular medications as normal with a sip of water.
What actually happens during the embolization?
We will get you comfortable lying on the image-guided operating table.
The nurse looking after you will give you an intravenous sedative to make you feel relaxed.
Your blood pressure, heart rate and oxygen levels will be monitored closely throughout the procedure.
The pelvic veins are actually accessed by a vein in the right side of the neck (jugular vein). The skin over the vein is cleaned and sterile drape placed over you.
Local anaesthetic will be injected through a fine needle under the skin and down to the vein, this will sting a little for about a minute and then go numb.
A small tube (less than 2mm in diameter) called a catheter will be carefully inserted into the vein under ultrasound guidance, once this is in position you will not really be aware of what is happening inside the veins.
The catheter is then manipulated under real-time low-dose X-ray into the pelvic veins.
The correct position of the catheter tip within the pelvic vein will be confirmed by injecting a dye which shows up on low dose X-ray.
Following this, small platinum coils are placed through the catheter into the pelvic veins. A sclerosant fluid is also injected around the coils. In combination the coils and sclerosant block the veins preventing back flow to the pelvis.
At the end of the embolization all tubes are removed. Pressure is applied to the side of the neck for 5 minutes to stop any bleeding from the access point.
Is the procedure painful?
The local anaesthetic at the beginning of the procedure stings a bit for around 60 seconds.
You may get a dull ache in the pelvis and tummy after the sclerosant is injected, which last for 10-20 mins, otherwise the embolization is not painful.
We will give you intravenous sedation throughout the procedure to keep you relaxed and comfortable.
What happens after the Embolization?
Once the embolization is completed, you will be transferred back to your private room on the ward for bed rest and observation for 2 hours. You can eat drink normally immediately after the procedure.
Before you go home, we ensure there is no bleeding from the vein access site. Some women will return to work the next day, however others may take a few days off, especially if they have very active jobs. You can return to sports and the gym after one week.
You will have our contact details if there are problems or you want to ask any questions.
Follow up after the PAE
Dr Burfitt will contact you by telephone 2 weeks after the PAE to see how you are doing.
Generally the discomfort from the pelvic congestion syndrome will resolve in the first month, but can take one or two more months.
Dr Burfitt will arrange a follow up outpatient appointment for 3 for months to review the outcome of the embolization.


